

pupil response for relative afferent pupillary defect (RAPD)ĭirect ophthalmoscopy alone is not enough as most retinal tears or detachment are in the periphery the patient should be referred to an ophthalmologist at this point.visual acuity of each eye separately and with glasses or pinhole.History: to help differentiate ocular from non-ocular causes of flashes and floaters ( Table 1).

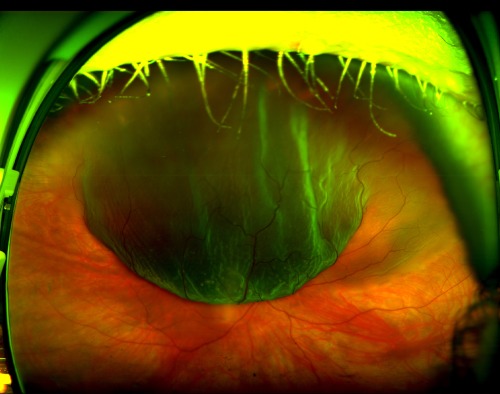
Exudative retinal detachment results from accumulation of fluid in the potential sub-retinal space due to disruption of hydrostatic forces (severe acute hypertension), inflammation or neoplasm. Tractional retinal detachment is caused by mechanical forces on the retina, usually as a result of previous haemorrhage, infection, inflammation, trauma or surgery. Other types of retinal detachment include tractional and exudative and these can also present with flashes and floaters. The most common location for a retinal tear is in the superotemporal quadrant (60%) and because of the effects of gravity results in a greater incidence of macula-off retinal detachment, compared with inferior or nasal retinal tears. Retinal detachment superiorly (optic disc visible in the background) 4,7Ī patient with posterior vitreous detachment is deemed to be at higher risk of retinal detachment if it is associated with vitreous haemorrhage about 70% of these patients have been found to have at least one retinal tear 8 ( Figure 1).įigure 3. Clinically, the patient has normal vision, no visual field defects and no relative afferent pupillary defect. During separation, the vitreous may tug and cause mechanical stimulation of the retina, resulting in flashes. 4,6 It is an age-related change in which the vitreous degenerates, shrinks and separates from the retina.
Posterior vitreous detachment (PVD) is the most common cause of acute onset of flashes and floaters, present in nearly 66% of patients over 70 years. They are more noticeable in dim lighting, may be triggered by eye movement and are usually in the temporal visual field. Flashes are typically described as a momentary arc of white light, similar to a bolt of lightning or a camera flash. Photopsias can be generated anywhere along the visual pathway, but in the eye they result from mechanical stimulation of the retina by vitreoretinal traction. 5įlashes are visual phenomena known as photopsias and refer to the perception of light in the absence of external light stimuli. The most common cause of vitreous haemorrhage is proliferative diabetic retinopathy. Floaters may also result from haemorrhage of retinal vessels into the vitreous and may be described as minute black or red spots. Patients may describe floaters as ‘flies’, ‘cobwebs’ or ‘worms’ that are more pronounced against light backgrounds.

4 Floaters may be caused by vitreous debris from infection, inflammation and haemorrhage, but are typically due to the age-related degeneration of the vitreous, forming condensations of collagen fibres. Floaters refer to the sensation of dark spots that are caused either by opacities in the vitreous, which cast shadows on the retina, or by light bending at the junction between fluid pockets and the vitreous.


 0 kommentar(er)
0 kommentar(er)
